For many, mirrors are a simple tool for grooming, a quick check before heading out the door. But for someone with Body Dysmorphic Disorder (BDD), a mirror can become a source of intense distress, reflecting a distorted reality that fuels a cycle of anxiety and shame. Body Dysmorphic Disorder is a serious mental health condition where a person becomes obsessed with perceived flaws in their appearance—flaws that are often minor or entirely invisible to others. Understanding the complex role mirrors play in this disorder is vital for those who suffer, their loved ones, and the clinicians working to help them heal.
This article will explore how mirrors influence Body Dysmorphic Disorder, delving into the psychological mechanisms that turn a simple reflection into a painful obsession. We will also discuss the profound emotional impact and, most importantly, the effective coping strategies and treatments that can help individuals reclaim their lives from the distorted image in the glass.
Understanding Body Dysmorphic Disorder

Body Dysmorphic Disorder is more than just feeling insecure about your appearance. It is a consuming preoccupation that can dominate a person’s thoughts and dictate their behaviors. Affecting an estimated 1.7% to 2.9% of the general population, BDD can impact anyone, regardless of age, gender, or background, though it often begins during adolescence.
The focus of this obsession can be any part of the body. Common areas of concern include the skin (acne, scars, wrinkles), nose (size or shape), and hair (thinning or excessive body hair). However, any feature can become the center of intense scrutiny, from the shape of one’s eyes to the size of their muscles.
Symptoms and Compulsive Behaviors
The distress caused by these perceived flaws drives a range of compulsive behaviors. These are not acts of vanity; they are desperate attempts to manage overwhelming anxiety. Key symptoms include:
- Excessive Mirror Checking: Repeatedly examining one’s reflection for hours each day, often focusing on the perceived defect. This can involve using multiple mirrors, magnifying glasses, or even reflective surfaces like windows and phone screens.
- Camouflaging: Trying to hide the perceived flaw with heavy makeup, specific clothing, hats, or by adopting certain postures.
- Comparing: Constantly comparing one’s appearance to that of others, both in person and on social media, which often reinforces feelings of inadequacy.
- Mirror Avoidance: In some cases, individuals may avoid mirrors and all reflective surfaces entirely to prevent the distress and anxiety that come with seeing their reflection.
- Reassurance Seeking: Persistently asking others if they notice the flaw or if they look “okay,” though any reassurance received provides only temporary relief.
These behaviors are accompanied by a heavy emotional toll. Individuals with BDD frequently experience profound anxiety, shame, disgust, and depression. The condition can be so debilitating that it leads to social isolation, difficulty functioning at work or school, and, in severe cases, suicidal thoughts and behaviors.
Causes and Risk Factors
Like many mental health conditions, BDD is believed to stem from a combination of factors. There is no single cause, but several elements can increase a person’s risk:
- Genetic and Neurological Factors: BDD tends to run in families, suggesting a genetic predisposition. Brain imaging studies have also shown differences in visual processing and serotonin systems in individuals with the disorder.
- Environmental Influences: Life experiences play a significant role. A history of childhood teasing, bullying, neglect, or trauma related to one’s appearance can contribute to the development of BDD.
- Societal Pressures: Living in a culture that places a high value on “perfect” looks, fueled by media and social media, can create and amplify body image dissatisfaction.
The Double-Edged Sword: Mirrors in BDD
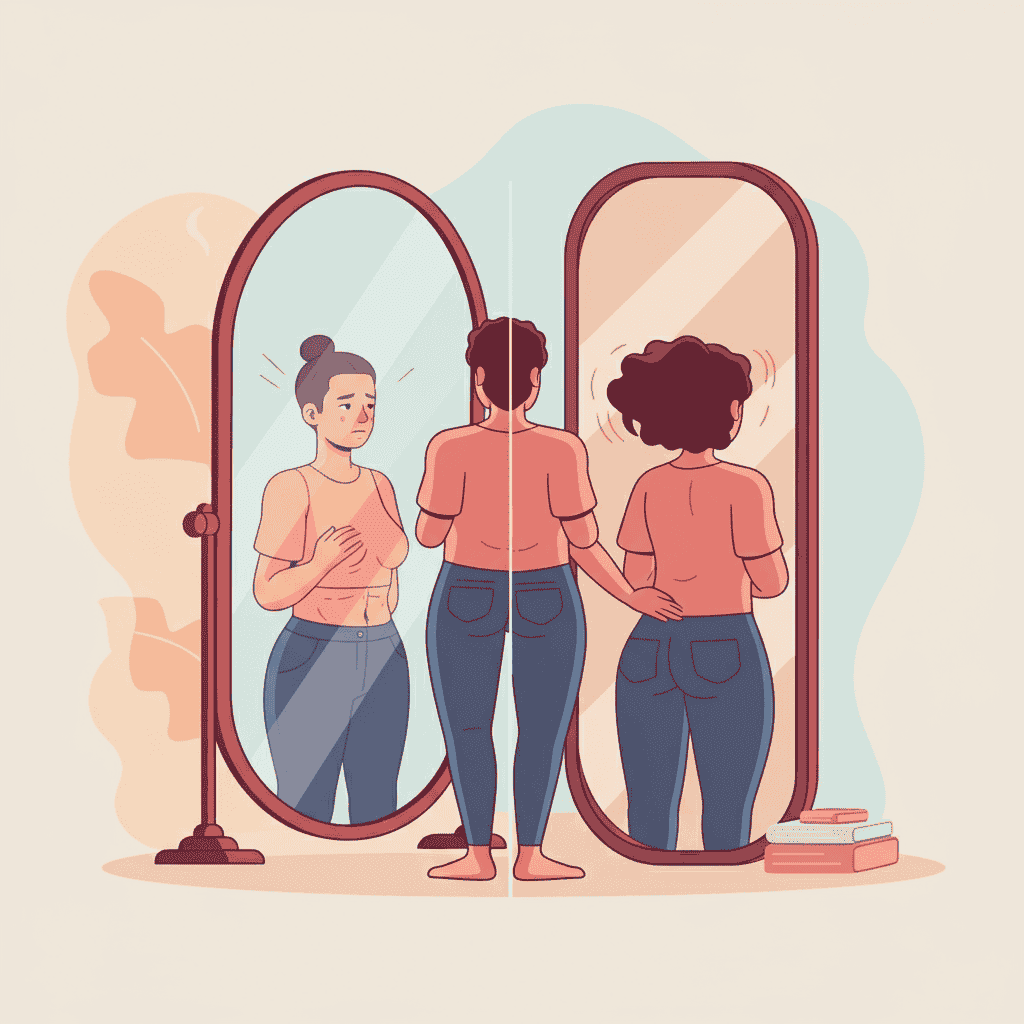
Mirrors are central to the BDD experience, acting as both a trigger and a tool for compulsive rituals. The relationship is often paradoxical, with individuals oscillating between obsessive checking and complete avoidance.
The Cycle of Mirror Checking
For many with BDD, mirrors are not a tool for objective self-assessment but a catalyst for obsessive scrutiny. This behavior often locks them into a painful “mirror loop”:
- The Check: An initial glance in the mirror triggers an intense focus on the perceived flaw.
- The Dissatisfaction: The reflection confirms and often exaggerates the perceived defect, leading to feelings of disgust and dissatisfaction.
- The Anxiety: This negative self-perception causes a spike in anxiety, distress, and shame.
- The Repeat: To try and alleviate the anxiety or to “check again just in case,” the person is compelled to return to the mirror, restarting the destructive cycle.
This loop can consume hours, trapping the individual in a state of heightened self-criticism and emotional pain.
The Paradox of Mirror Avoidance
While some are drawn to the mirror, others go to great lengths to avoid it. They might cover mirrors in their home, get ready in the dark, or avert their gaze from any reflective surface. This avoidance is a protective mechanism—an attempt to escape the crushing distress that seeing their reflection brings. This behavior, while different from checking, is equally disruptive and reinforces the belief that their appearance is too horrible to be seen.
Psychological Mechanisms at Play
Several psychological processes explain why mirrors are so problematic in BDD:
- Distorted Self-Perception: Individuals with BDD do not see themselves as others do. Their brain’s visual processing appears to be altered, leading them to genuinely perceive exaggerated flaws. They may focus on minute details while losing sight of their appearance as a whole.
- Cognitive Biases: Selective attention causes them to zero in on their “bad” spots while ignoring all other features. Confirmation bias leads them to interpret any ambiguous reflection as proof of their defectiveness.
- Reinforced Dissatisfaction: Each time they engage with a mirror and feel distress, the connection between their reflection and negative emotions is strengthened, solidifying their poor body image.
Research supports these ideas. Studies using mirror exposure have found that individuals with BDD experience a significant increase in distress and negative self-perception compared to control groups, confirming that mirrors are a powerful trigger for symptoms.
The Emotional and Social Fallout
The constant battle with one’s reflection has devastating consequences that ripple through every aspect of life. BDD is not a superficial concern; it is a disabling condition with serious mental health implications.
The relentless focus on appearance and the associated compulsive behaviors frequently lead to severe anxiety, clinical depression, social withdrawal, and dangerously low self-esteem. The shame and fear of judgment can make it nearly impossible to engage in social activities, leading to profound isolation.
Relationships with family and friends can become strained. Loved ones may struggle to understand the severity of the distress, and the constant need for reassurance can be draining. The time consumed by rituals can also interfere with shared activities and responsibilities. This isolation further impacts daily functioning, making it difficult to maintain a job, succeed in school, or even leave the house.
Strategies for Healing: Coping and Treatment
Despite the severity of BDD, there is hope. Effective treatments and coping strategies can help individuals break free from the cycle of obsession and improve their relationship with their reflection and themselves.
Therapeutic Interventions
Cognitive Behavioral Therapy (CBT) is the gold-standard treatment for BDD. A specific form of CBT called Exposure and Response Prevention (ERP) is particularly effective for addressing mirror-related behaviors. In ERP, a therapist guides the individual in gradually confronting their fears (exposure) without engaging in their usual compulsive rituals (response prevention).
For mirror use, this might involve:
- Starting with brief, timed glances in the mirror.
- Looking at one’s whole reflection from a distance rather than focusing on specific parts up close.
- Resisting the urge to camouflage or perform checking rituals after looking in the mirror.
The goal is not to force someone to “like” what they see, but to reduce the anxiety and break the compulsive cycle associated with mirrors. Over time, this helps the brain learn that the feared outcome does not occur, and the anxiety subsides.
Practical Strategies for Mirror Use
Alongside therapy, individuals can practice practical strategies to manage their mirror use:
- Limit Mirror Time: Use a timer to keep mirror use brief and purposeful, such as for shaving or applying makeup.
- Reduce the Number of Mirrors: Cover or remove unnecessary mirrors in the home to reduce temptation.
- Practice Mindful Observation: When looking in the mirror, try to describe what you see factually and non-judgmentally (“I see my face, I see my eyes”) rather than critically.
- Challenge Negative Self-Talk: Actively work to stop the stream of critical thoughts in front of the mirror. Replace harsh judgments with neutral or compassionate statements.
Medical and Support Systems
Medications, particularly Selective Serotonin Reuptake Inhibitors (SSRIs), can be very effective in reducing the obsessive thoughts and compulsive behaviors of BDD. They are often used in combination with therapy for the best results.
A strong support system is also crucial. Educating family and friends about BDD can help them provide understanding and encouragement rather than unhelpful reassurance. Support groups, either in-person or online, connect individuals with others who truly understand the struggle, reducing feelings of isolation.
Wider Societal and Cultural Context
It’s impossible to discuss BDD without acknowledging the societal pressures that contribute to it. We are surrounded by images of unrealistic beauty standards in advertising and on social media platforms. These digitally altered and curated images create a distorted sense of what is normal and attractive, putting immense pressure on individuals to achieve an impossible ideal.
While BDD is a clinical disorder, promoting media literacy and a healthier, more diverse definition of beauty from a young age can serve as a powerful preventive measure. Fostering body positivity and self-worth based on character, skills, and kindness—rather than appearance—can build resilience against these harmful societal messages.
Conclusion: Finding Peace Beyond the Reflection
Mirrors in Body Dysmorphic Disorder are not just reflective glass; they are powerful amplifiers of internal pain, capable of trapping individuals in a cycle of obsession and despair. However, by understanding the psychological mechanisms at play, we can see that the problem is not the reflection itself, but the distorted interpretation driven by BDD.
With the right interventions, such as CBT and ERP, individuals can learn to neutralize the power of the mirror. By developing new coping strategies and challenging negative thought patterns, they can reduce their compulsive behaviors and lessen their emotional distress.
There is immense hope. Through therapy, support, and self-compassion, someone with BDD can change their relationship with their reflection. They can learn to see themselves beyond the perceived flaws and find a sense of peace and self-acceptance that is not dependent on what the mirror shows.